A new clinical trial suggests magnesium supplements may boost gut bacteria that help block the development of colon cancer – but only for some people, depending on their genes and sex.
An increase in the use of colonoscopies as a surveillance tool has reduced the incidence of colorectal cancer. However, despite this, it remains the third most common cancer globally, and the second leading cause of cancer-related deaths worldwide.
New research led by the Vanderbilt University Medical Center (VUMC) has demonstrated, by way of a clinical trial, that magnesium supplements increase gut bacteria that can inhibit the growth of colorectal cancer.
“Our previous study showed magnesium supplementation increased blood levels of vitamin D when vitamin D levels were low,” said Qi Dai, MD, PhD, professor of medicine at VUMC and the study’s corresponding author. “The current study reveals that magnesium supplementation also increases the gut microbes which have been shown to synthesize vitamin D in the gut without sunlight and locally inhibit colorectal cancer development.”

Sunlight is the body’s main source of vitamin D, which is essential for strong bones and overall health. Previous studies have found a link between vitamin D deficiency and colorectal cancer. In the current study, which was a double-blind randomized controlled trial, the researchers recruited 240 participants with a history of colorectal polyps, a risk factor for colorectal cancer. People were randomly assigned to take either personalized magnesium supplements or a placebo for 12 weeks. The dose of oral magnesium (magnesium glycinate) given was based on participants’ calcium-to-magnesium intake ratio, which is generally considered to be around 2:1 calcium to magnesium on a weight basis.
The researchers collected stool samples, rectal swabs, rectal tissue, and blood samples before and after the intervention. They looked at two gut bacteria – Carnobacterium maltaromaticum and Faecalibacterium prausnitzii – that have previously been shown in mice to help produce vitamin D in the gut and reduce cancer development. They also tested whether genetic differences in the TRPM7 gene, which is important for magnesium regulation in the body, changed the effects of supplementation. TRPM7 can be thought of like a “magnesium gate” in the cells. If the gate isn’t working properly, magnesium levels in the body and in the gut may not be well-regulated.
Before discussing what the researchers found, it’s necessary to talk briefly first about genetic variations. Here, the researchers were on the lookout for what’s called a “missense variant.” The genetic code in DNA is written in “letters”, and sometimes a single letter changes, which is called a variant (or mutation). A missense variant means that this tiny DNA change swaps one amino acid building block for another. In TRPM7, the study looked at a missense variant where the protein’s 1482nd position changes from one amino acid (threonine) to another (isoleucine). This is a bit like swapping one piece in a lock-and-key system: the protein still works, but maybe not as smoothly.
What the researchers found was that people without the TRPM7 missense variant (normal TRPM7) responded well to magnesium. It increased the abundance of C. maltaromaticum and, to a lesser degree, F. prausnitzii. This increase was strongest in women, suggesting that hormones like estrogen might play a role. In participants with the TRPM7 missense variant (Thr1482Ile), magnesium sometimes had the opposite effect, reducing these bacteria. The extra bacteria didn’t explain increases in vitamin D, though, which suggested that magnesium works on vitamin D metabolism both directly and through the microbiome, but via separate mechanisms.
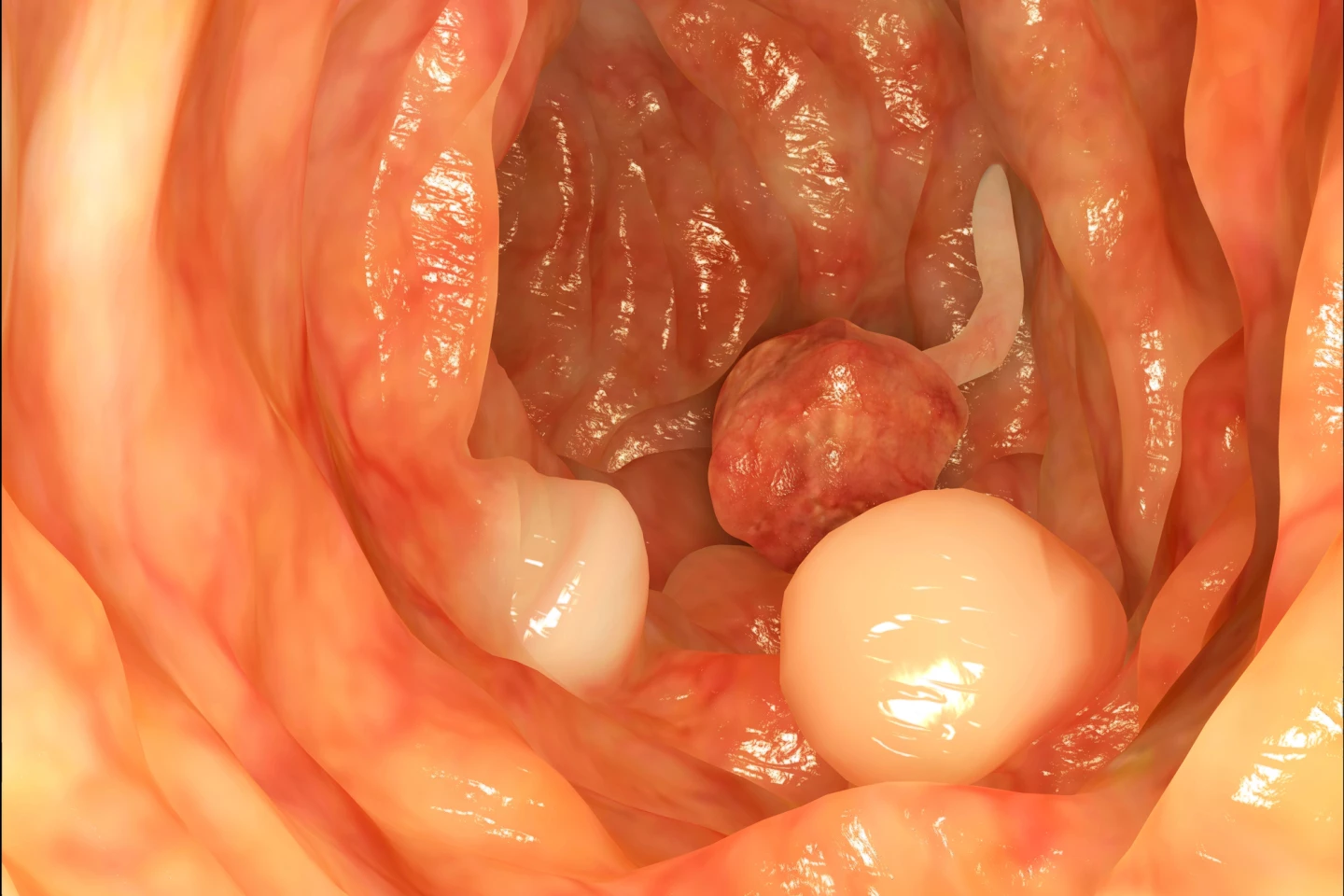
Exploratory follow-up colonoscopies found that in rectal tissue biopsies, people with the highest levels of F. prausnitzii had about a 2.8-fold (nearly three times) higher risk of developing new polyps compared to those with the lowest levels. This association was statistically significant. Whereas, higher levels of C. maltaromaticum were linked to approximately an 85% lower risk of developing serrated polyps, which are less common than conventional polyps but are associated with an increased risk of colorectal cancer and may progress faster when they do become cancerous. However, this result was only “marginally significant,” so it should be seen as suggestive rather than conclusive. In stool samples, neither bacterium showed a clear or consistent link with polyp risk.
The study had limitations. The increase in F. prausnitzii did not remain statistically significant after correcting for multiple comparisons, so results should be interpreted cautiously. The study didn’t identify which strains of bacteria were responsible, and effects may vary by strain. Microbial changes were measured in relative abundance (percent of total bacteria), which may shift even if absolute numbers of bacteria don’t. Participants were mostly older, White, and from a single geographic area (Tennessee, US), so results may not generalize widely. Finally, the trial was relatively short (12 weeks), so long-term effects are unknown.
Nonetheless, the research suggests that magnesium supplementation may help to prevent colorectal cancer, especially in women and in people without certain TRPM7 genetic variants. This suggests a possible “precision nutrition” strategy, where genetic testing could guide who benefits most from taking magnesium. However, more research is needed before this can be turned into clinical advice.
The study was published in The American Journal of Clinical Nutrition.
.png)


