Jun 11, 2025
Biomarker-driven nutrition: how to go beyond generic diet advice
“Eat less sugar.” “Eat more leafy greens.” “Eat whole grains.” These generic nutrition tips are everywhere. What if we could give more precise dietary advice, based on your specific biomarkers?
It turns out, we can. Biomarker-driven nutrition plans are well-supported by medical research, which deserves to be better known.
For example, one landmark randomized control trial showed an 11.4 mmHg decrease in systolic blood pressure from a high-potassium diets. A follow up showed an additional 3.0 mmHg drop from a low sodium variation of this diet, with a graded effect:
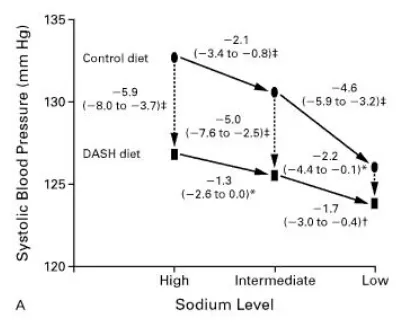
This is significant! Every 5 mmHg reduction in systolic blood pressure reduces the risk of major cardiovascular events by about 10% (study). Additionally, each 20 mmHg reduction in systolic blood pressure can lower the risk of cardiovascular disease (CVD) by nearly 50% (study).
The rest of this post will discuss biomarker-driven nutrition,
First, let’s define the biomarkers we care about—they’re the ones that predict your heart attack risk. Namely:
- High blood pressure
- High LDL cholesterol or ApoB
- High A1c (blood sugar)
- Low HDL cholesterol (or Apo A1)
A good place to start if you want to reduce your blood pressure through nutrition is the DASH (Dietary Approaches to Stop Hypertension) diet. Originally, the research found that a diet high in healthy foods like fruits and vegetables, whole grains, nuts, legumes, and lean proteins like chicken and fish and low in saturated fats, red meats, and sugar led to a significant reduction in blood pressure. But further research showed that reducing sodium intake and increasing potassium intake can have additional positive effects on reducing blood pressure. The study showed that reducing sodium resulted in a 7.1 mmHg lower blood pressure compared to those on a high sodium diet
How nutrients drive specific biomarkers like cholesterol and blood pressure
Each biomarker is driven by specific nutrients in your diet. Which nutrients you should focus on depends on your blood test results. If your LDL is high but your blood pressure is normal, you’d focus on different dietary changes than someone with high blood pressure but normal cholesterol.
Here’s a simplified guide to biomarker-driven nutrition:
| High LDL (or ApoB) | Fiber, good fats | Saturated fat (for some) [1] |
| High blood pressure | Potassium | Sodium |
| High A1c | Fiber | Refined carbs or sugar |
| Low HDL | Good fats | - |
Now, let’s apply this to a real-world example.
How biomarker-driven nutrition let you make real-world tradeoffs about meals
Let’s take an example of three meals from a “healthy bowls” restaurant. Any of these should be good for heart health, right?
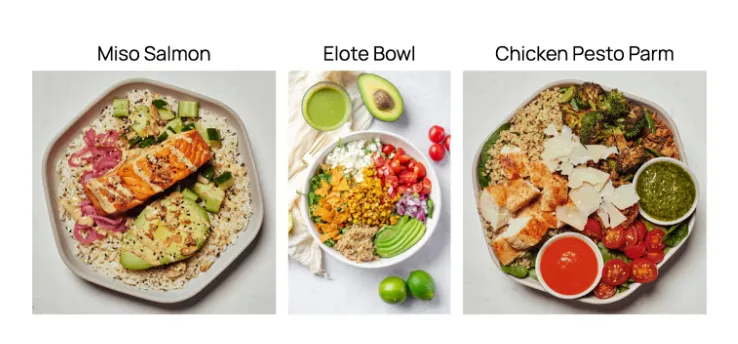
Wrong. It actually depends on your biomarkers. Trying to lower LDL? The chicken pesto parm healthiest: 9g of fiber for only 3g saturated fat. If you’re trying to raise HDL, it’s the reverse. If you’re trying to lower blood pressure, the elote bowl has about 40% less sodium than the miso salmon and 45% less than the chicken pesto parm (the miso salmon is the worst option: at 1272 mg sodium, one meal alone is 85% of your daily allowance without much potassium). But how would you know all this just by looking at the meals?
Tracking nutrients through food photos
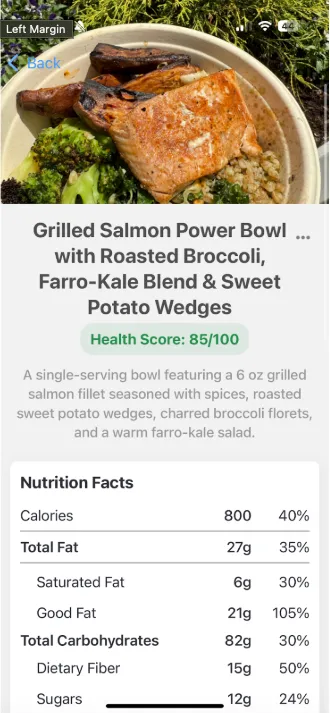
That’s where Empirical Health comes in. Based on my personal biomarkers, my doctor at Empirical Health told me that I should try to lower ApoB and blood pressure to improve my heart health. Therefore, I need to lower my sodium intake and increase my potassium and fiber.
Want to try it? Download Empirical Health for iOS or Empirical Health for Android today.
Notes
[1] The original DASH trial, published in 1997, compared two potassium-rich diets with a normal diet. The DASH-sodium trial, published in 2001, measured the gradient of blood pressure with respect to sodium, while keeping potassium intake constant. OmniHeart subsequently explored the effects of different macronutrients.
.png)



